 New Health Guide
New Health Guide
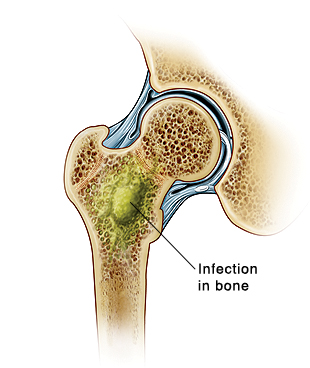 Osteomyelitis is the inflammation of the bones. The infections of bones spreading from neighboring tissues or traveling in the bloodstream. Alternatively, if an injury directly exposes the bone to microorganisms, osteomyelitis can originate in the bone itself.
Osteomyelitis is the inflammation of the bones. The infections of bones spreading from neighboring tissues or traveling in the bloodstream. Alternatively, if an injury directly exposes the bone to microorganisms, osteomyelitis can originate in the bone itself.
In adults, osteomyelitis most frequently affects the vertebrae, whereas in children, the condition is more common in the long bones of the arms and legs. Diabetics who have foot ulcers are susceptible to osteomyelitis in the feet. Common symptoms of osteomyelitis include pain, swelling, warmth and redness in the area of infection, also fevers and chills. Although osteomyelitis was previously considered to be incurable, nowadays there are a variety of treatment methods available.
The primary aims of osteomyelitis treatment are to stop the infection and to prevent the development of chronic infection, which can result in permanent deformity, possible fractures and other chronic issues. Therefore, it is essential to treat the osteomyelitis as quickly as possible. Osteomyelitis patients are usually hospitalized and treated with a combination of antibiotics and surgery.
The type of infection causing the osteomyelitis will usually be diagnosed using a bone biopsy. Once the cause of the infection is identified, your doctor will select the correct osteomyelitis antibiotics, which are given to you through intravenous injection via an arm vein for 4-6 weeks or longer. You usually receive these injections as an outpatient, so you can return home the same day. During the treatment, you may experience side-effects, such as nausea, diarrhea and vomiting.
An additional course of oral antibiotics could be required once your symptoms improve. Effective oral antibiotics for the treatment of osteomyelitis include rifampin, clindamycin, trimethoprim-sulfamethoxazole, and fluoroquinolones. These are often administered in combination as dual therapy. In certain cases, the bacteria causing the osteomyelitis have developed resistance to some of the antibiotics; in this situation, less frequently used antibiotics may be needed.
One or more of the following surgical operations may be performed to treat the osteomyelitis, depending on the extent of the infection:
If the osteomyelitis does not respond to conventional treatment, hyperbaric oxygen therapy, a non-surgical osteomyelitis treatment, may be considered. During this procedure, the patient is placed in a specially designed chamber, similar to decompression chambers employed by divers. Oxygen, at a markedly higher pressure than usually found in the atmosphere, is then fed into the chamber. This procedure is thought to promote healing and halt the spread of infection, although the evidence supporting hyperbaric oxygen therapy for osteomyelitis treatment is limited. It seems to be most effective in treating osteomyelitis originating from diabetic foot ulcers, although this is currently only recommended for use in clinical trials.
The prognosis for patients with osteomyelitis depends greatly on the patient’s general health and their risk factors. If the patient receives prompt diagnosis and treatment, a complete recovery can be achieved, although they will have to be closely monitored over the next few months in case a relapse occurs. The best results are seen in patients who receive treatment within 3-5 days after the initial infection.
The best way to prevent osteomyelitis is to keep all injury sites clean. Wash all cuts, particularly deep cuts, thoroughly, rinsing any open wounds under running water for at least 5 minutes before wrapping the injury in sterile bandages.
If you do develop osteomyelitis, get treatment as soon as possible. The earlier osteomyelitis is addressed, the better the chance of recovery, and the lower the likelihood of it developing into a chronic condition.
In cases of chronic osteomyelitis, consult your doctor about how to best manage the condition, ensuring that he or she has your complete medical history. For diabetics, it is important to look after your feet, and to contact a medical professional if you see any sign of infection.