 New Health Guide
New Health Guide
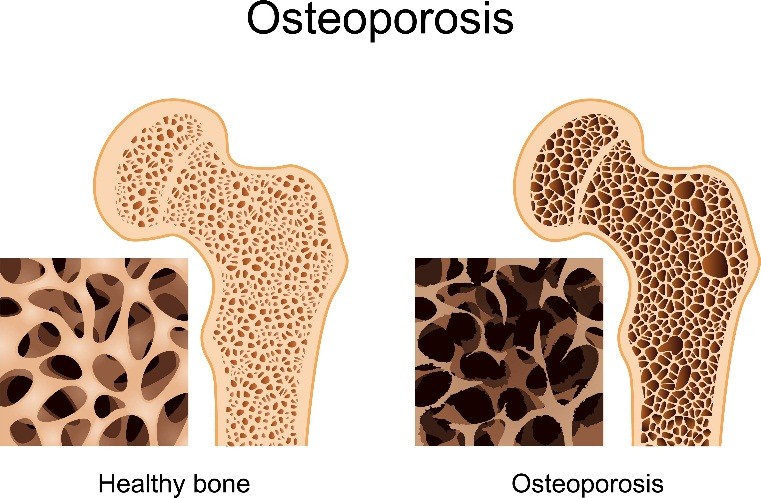
Osteoporosis is a bone condition where there is a decrease in the density and strength of bones, resulting in fragility. Osteoporosis leads to porous bones that make them compressible, just like sponge. This skeletal disorder weakens bones, which results in frequent breakage or fractures in the bones. A similar condition, called osteopenia, is a condition where bones are less dense than normal, but not to the same degree as osteoporosis.
The bones are composed of calcium, protein, and collagen, which give bones their structure and strength. With osteoporosis, bones can break or fracture easily, even with minor injuries that normally do not cause fractures. These fractures can be in the form of cracks (such as in hip fractures), or bones may collapse (such as compression fractures of the spinal vertebrae). Fractures related to osteoporosis can affect any bone, but those of the spine, ribs, hips and wrists are most common.
 Osteoporosis may not cause any symptoms in the early stage of the disease. However, it may later cause dull pain, especially in the neck or in the lower back. Still later in the course of this disease, one may develop sudden onset of sharp pains. Pain may not spread or radiate to other areas, but it may become worse with activity, or when one puts weight on the affected area. This may also be accompanied by pain on touch, or tenderness, which may subside within one week. Pain, however may last more than 3 months.
Osteoporosis may not cause any symptoms in the early stage of the disease. However, it may later cause dull pain, especially in the neck or in the lower back. Still later in the course of this disease, one may develop sudden onset of sharp pains. Pain may not spread or radiate to other areas, but it may become worse with activity, or when one puts weight on the affected area. This may also be accompanied by pain on touch, or tenderness, which may subside within one week. Pain, however may last more than 3 months.
Fracture in the hip or wrist may follow a fall, but in other cases, people who have osteoporosis do not recall any trauma or fall that may cause a fracture in other parts of the body such as the spine. A stooped posture and a reduction in height may result from a spinal compression fracture due to osteoporosis.
Talk to your doctor about the possibility of bone weakness if you have a family history of osteoporosis, especially hip fractures. You may also be a candidate for the condition if you had an early menopause, or if you took treatments with corticosteroids for several months.
The bones are constantly being renewed as old bones are broken down and new bones are formed. While you were young, the body new bone is made faster than old bone is broken down, so that bone mass is increased. Bone mass reaches its peak by the time you are in your early 20s. However, as you age, you lose bone mass faster than you make new bone.
Various factors increase the risk of osteoporosis, and these include the following:
|
Risk Factors of Osteoporosis |
|
|
Non-Modifiable Risk Factors |
|
|
Modifiable Risk Factors |
|
|
Medication Risk Factors |
|
These include bisphosphonates such as
2. Less Common Osteoporosis Medications
These are used if you cannot tolerate common drugs for osteoporosis:
3. Hormone-Related Therapy
Regular exercise for at least 30 minutes about five times a week helps prevent osteoporosis by stimulating bone production and strengthening your bones. Weight-bearing exercises are best, and these include brisk walking, dancing, running, and aerobics. Older people may benefit from regular walking.
Exercises that strengthen the muscles are also important to support the bones, improve balance, and prevent falling. Examples include weight lifting and press-ups.
Watch the video to know how to prevent Osteoporosis by spine strengthener exercise:
Experts recommend taking at least 1,000 mg of calcium, and at least 800 IU of vitamin D per day, for people older than 50. You must also take at least one gram of protein per kilogram of body weight per day.